Disagree the studies are not good. Pull the restrictions off and let doctors and patient decide.
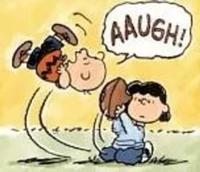
You will say that about every study that lacks evidence forHCQ efficacy. That’s the problem. Reminds me of Lucy and the football:
I have said what I have it will come out what happened in the general public with the steroids and then those Respinsible will have to explain why so many could have been saved and if eventually hcq is shown effective early or to prevent longhaulers then what?
Anyways enough said. it may be interesting that the hcq interferes with malaria which binds the cd 147 molecules the same target for for the cvd 19 spike protein.
The data shows that it isn’t effective. What do we do when people refuse to accept the data?
Worked for opiates, should work for Covid treatments. ![]()
A risk ration of 0.49 means that it was effective for over half the participants.
You forgot the error bars.
So when Professor Risch said, “ For those patients, the medications cut the risk of a bad outcome in half,” you’re saying he didn’t know what he was talking about.
For those patients, the differences between treated and control were not statistically significant. That’s what the conclusions of the paper are. When someone makes a claim that isn’t supported by the paper then that person doesn’t know what they are talking about. Means are meaningless without statistical analysis.
I suspect that the differences for the nursing home residents were not considered significant, because there were only 133 treated residents, and only 67 or so had positive outcomes, which would be statistically insignficant if included in a study of roughliy 2,000 participants.
But if you think that Professor Risch does not know how to read and interpret these graphs, I think you should report it to the Yale School of Public Health. Perhaps they’ll make sure he takes a remedial course.
Now what might make these numbers more significant is knowing how many days after exposure the nursing home residents were treated. Of course, it would help if they broke it down into day 1, day 2, day 3, etc, instead of just giving us three groups.
It’s not my job to police Risch’s actions.
The conclusions become meaningless if you have to whittle the data down like that. At that point you are chasing significant differences instead of testing hypotheses.
I didn’t see anywhere in the hypothesis that they insisted that they could only measure in three different groups of days. Why would that be important? We are testing post exposure prophyhlaxis, afterall. So perhaps the sooner the better (which is what the results of their groupings suggest). That’s what Watanabe’s re-analysis of Boulware’s study suggested. I suspect somebody will suggest they do the same for the Barcelona study. Let’s divide the treated into six equal parts, one for each day. So 22 treated per day. The first day 21 are effectively protected. The second 18. The third 14. The fourth 10. The fifth 3. The fifth 1. The sixth 0. I’m not sure what that would do to the stats, but it sure looks suggestive to me.
That’s what happens when doctors don’t have good data to guide them about which drugs to use. All kinds of claims about all kinds of treatment have been made. Is your position that every one of those treatments should have been used?
The WHO saw data of ineffectiveness – the same data that caused doctors at Mass General to stop using, among many others.
Anything that doesn’t outright kill patients might be effective. That’s a terrible basis for deciding what treatments to use.
I agree about the politicization – but having a president of the US pushing an untested drug will have that effect. As for blemishes, having the FDA offer any kind of endorsement of HCQ without good evidence was a blemish.
It is interesting that Dr. Risch deals mostly with cancer, and not infectious disease. His fellow Yale docs in epidemiology are not so supportive either. I’ll call your doc, and raise you twelve:
Such a good quote. These are difficult times, and many of us want to help where we think we can. However, sometimes we forget our expertise.
Dr Oz, a respected cardiothoracic surgeon, reportedly makes only 46% or so of his recommendations with good internal medicine basis (such as saying GMO causes cancer). https://journalofethics.ama-assn.org/article/case-dr-oz-ethics-evidence-and-does-professional-self-regulation-work/2017-02
I have to look at the study on dexamethasone again, but the actual improvement in absolute numbers in mortality, since it was only in those intubated, seems less than one would expect. A wild card seems to be whether asthma or steroid-responsive COPD is a factor. CDC recommends treating asthma and COPD appropriately with steroids (inhaled vs intravenous) whether patients have Covid or not. Asthma can be mild intermittent and evident only with infections or other stimuli, so I’m not sure if the improvement is more limited to those with asthma (previously known or not), and whether it would even have helped with those without asthma. It’s a messy area, and steroid use in ICU sepsis has been controversial in the last few decades more than once.
Dr. Risch made it clear that nothing his Yale colleagues said was relevant to the points that he had made. Maybe if you read his articles and compared it with what they wrote, you would see that.
Nowhere in the hypothesis did it state they were looking for a specific effect in a specific group on a specific day.
Where is there any data demonstrating earlier treatment reduces development of disease?
But they break down the results into three time periods: 1-3 days, 4-6 days, and 7 or more days. Why? And if they are willing to break it down into those groups, why not break it down into smaller groups, such as each day? Wouldn’t it be useful to know if HCQ works very well on day 1 or 2, but not so well after that?
Why not break it down to the hour, or the minute? At some point it is meaningless because disease progression may not be consistent to the minute, hour, and day.
It is interesting, but most important would be mortality outcomes. I’m puzzled, as he responds to their critique only in small areas–where it is really hard to say if anything helps or not. I’m surprised he alludes to his multiple publications in cancer as reason to trust his judgment.
If I had great approval from my patients for primary care, it’s not a reason for someone to trust my judgement in assessing chemotherapy outcomes.